The IoMT Dilemma: Securing Legacy Medical Infrastructure Without Disrupting Care

In the modern clinical environment, the Internet of Medical Things (IoMT) is both a miracle of patient care and a nightmare for security practitioners. From infusion pumps to MRI machines, these devices provide real-time data that saves lives. However, many are built on “zombie” operating systems—Windows XP or early Linux kernels—that cannot be patched, updated, or even scanned without risking a system crash.
For senior security consultants, the challenge isn’t just “securing the network.” It is securing the network while ensuring that a lifesaving ventilator never loses connectivity.
The Reality of Legacy “Clinical Debt”
In any other industry, an unpatchable Windows 7 workstation is a liability to be replaced. In healthcare, that workstation might be the $2M proprietary interface for a linear accelerator used in oncology. You cannot simply “turn it off.”
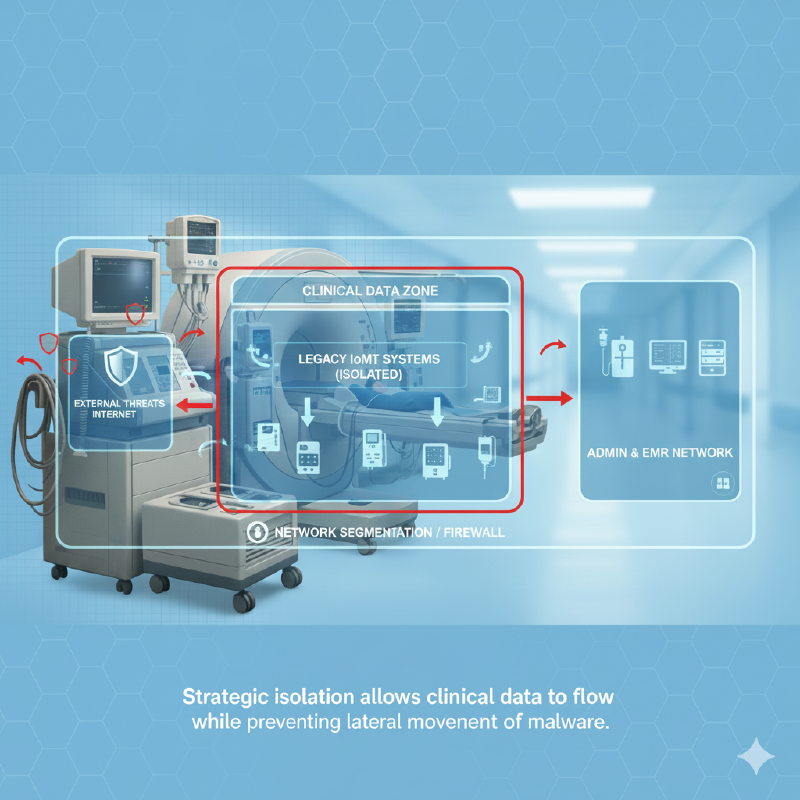
This creates Clinical Debt: the accumulation of security vulnerabilities that are intentionally accepted to maintain patient outcomes. Securing this environment requires moving the defense from the endpoint to the network architecture.
1. Zero-Trust Micro-Segmentation: The “Virtual Bubble”
The most effective tool in the consultant’s arsenal is Micro-segmentation. Rather than relying on a single “Clinical VLAN,” we wrap legacy devices in virtual bubbles.
- The Principle of Least Privilege (Network): An infusion pump needs to talk to the central monitoring station and perhaps a time server. It does not need to talk to the hospital’s guest Wi-Fi, the billing department, or the internet.
- Enforcement: Using Software-Defined Networking (SDN), we create “Micro-perimeters.” If an attacker compromises a laptop in the HR department, the segmentation prevents them from even “seeing” the life-support systems on the network.
2. Managing the “Scanner’s Dilemma”
Traditional vulnerability scanners (like Nessus or Qualys) work by sending “probes” to devices. While a modern laptop handles these easily, a 15-year-old medical device might interpret a port scan as a command to reboot or freeze.
The Consultant Approach:
- Passive Discovery: We utilize passive traffic analysis tools (like Claroty or Ordr) that “listen” to network traffic rather than “shouting” at devices.
- Device Profiling: We build a “Digital Twin” of the device’s expected behavior. If a heart monitor suddenly starts communicating via an encrypted SSH tunnel to an offshore IP, we don’t need a scan to know it’s compromised.
3. The “Containment First” Incident Response
When a legacy medical device is suspected of infection, the standard “wipe and reload” IT protocol is often impossible. The software may no longer be supported by the vendor, or the calibration settings may be lost.
Consultants focus on Traffic Shunting. Instead of taking the device offline, we apply an immediate network ACL (Access Control List) that allows the device to continue its clinical function (sending vitals to a nurse’s station) while blocking all other lateral movement. This buys the clinical team time to transition the patient to a backup device safely.
4. Bridging the Gap: IT vs. Biomed
The greatest vulnerability in hospital security isn’t technical—it’s organizational. The IT team often doesn’t understand the clinical urgency, and the Biomedical (Biomed) team doesn’t always understand the cyber risk.
Senior consultants act as the “Clinical Translator.” We align security controls with Patient Safety. We don’t frame segmentation as a “compliance requirement”; we frame it as a “high-availability requirement” to ensure the device is available when a patient needs it most.
Strategic Mitigation Checklist for 2026:
- Inventory Accuracy: You cannot secure what you cannot see. Maintain a real-time, hardware-level inventory of all IoMT assets.
- VLAN Decoupling: Move away from “flat” networks. Isolate imaging, telemetry, and administrative traffic.
- Manufacturer Disclosure Statement for Medical Device Security (MDS2): Always demand the MDS2 from vendors to understand exactly what protocols the device uses before it hits your wire.
- Legacy Wrapper: For devices that must remain on the network, use a “Security Gateway”—a small hardware firewall placed physically between the device and the wall jack.
Resilience Over Perfection
Securing legacy medical infrastructure is not about reaching a “state of zero risk.” It is about Resilient Engineering. By assuming the device is vulnerable and building the security around it, we protect the patient without ever interrupting the care.